When I was chatting with a friend about what happened in the hospital after the baby was born, she said that the doctor asked her if she wanted to circumcise the baby?
I’m wondering why my doctor didn’t ask me! When the baby was born and was still in the hospital for a few days, I was busy breastfeeding every day, and the baby also had a lot of examinations to do. I didn’t think about it at all! If the doctor doesn’t ask, who would have thought about it? I thought to myself, if I asked, maybe I would decide to do this operation before I was discharged from the hospital: the baby ate and slept, slept and ate, and had no mobility. It should be easier to recover (care).
Later, I had the opportunity to ask an Australian pediatrician. She said that, like China, Australia does not advocate circumcision of newborns, because Australian medical experts commented that the risks outweigh the benefits when the circumcision is performed for non-medical reasons. And Australia’s public hospitals will not circumcise boys unless there is a medical reason.
This seems to be different from what I know is common practice in American hospitals. I searched for the opinion of the American Academy of Pediatrics on this issue before, and found that doctors in the United States will discuss this issue with mothers during pregnancy, and many male babies have this operation at birth.

I’ve always wondered why the American Academy of Pediatrics, which has always been evidence-based, advocates circumcision of newborns, but China and Australia don’t?
Two years ago, I asked a urologist about it, and his opinions are also representative:
“The age of children’s circumcision, I personally think 5-7 years old is the best, because children are basically sensible and can cooperate with local anesthesia. But the biggest advantage is that after the vigorous development of puberty, the pigment differences and surgical marks on the inner and outer plates are almost invisible in the mature penis.”
Recently, a friend of mine’s baby also consulted a urologist because of repeated balanitis, whether he needs circumcision. The advice is still that the baby’s condition is not yet medically qualified to require surgery, and you can see a dermatologist first.
To be honest, my mind is also full of question marks: Why does the American Academy of Pediatrics advocate and we do not advocate circumcision of newborns? What medical indications should I “observe” for circumcision?
After checking the literature again, the question in my heart was finally answered.
Circumcision has a long history, especially the “circumcision” of male newborns, which is a very sacred ceremony in the eyes of Jews and Muslims.
This religious circumcision is controversial. In Cologne, Germany, in May 2012, the district court sentenced a surgeon for circumcising an Islamic boy aged 4.
However, in December of the same year, a Bill submitted by the Merkel government reconfirmed the legality of religious circumcision, allowing people to circumcise boys according to their own customs.

In the United States, a circumcision country, circumcision is usually performed shortly after the birth of a newborn.
The American Academy of Pediatrics (AAP) even formed a panel in 2007 to review nearly 40 years of medical research on circumcision to assess the medical benefits, advantages, and risks of circumcising newborns (boys).
In 2012, the American Academy of Pediatrics updated its policy statement on circumcision, declaring that the benefits of circumcising a newborn outweigh the risks.
This report lists many benefits of circumcising a newborn, and the risk of infection from circumcision in the United States is very low. The report also pointed out that the decision of parents to “cut” for their children is justified because of the many benefits.

The recommendations of the American Academy of Pediatrics tend to favor mutilation in the neonatal period if possible, on the grounds that:
- The greatest cumulative benefits of circumcision are obtained during the neonatal period: circumcision reduces urinary tract infections, penile cancer, and STD risk.
Especially for reducing urinary tract infections, that is “early cut and early enjoyment”. Studies have shown that urinary tract infections are high in the first 6 months of life, and that urinary tract infections in newborns may cause kidney damage with serious consequences. UTIs in uncircumcised boys range from 1% to 4%, compared with 0.1% to 0.2% for circumcised boys.
But in fact, it can be seen from this data that the absolute risk of urinary tract infection in male infants is relatively low.
- The data show that if not done in the neonatal period, the probability of doing it later is lower, and there is no benefit from not doing it: “Men who were born uncircumcised were much less likely to choose circumcision in adolescence or early adulthood. It should clearly inform parents who are considering postponing circumcision that circumcision later in life increases risks and costs.”
- In addition, neonatal circumcision is safer (fewer complications), simpler, and heals faster and better than subsequent circumcision.
Note, the American Academy of Pediatrics also states that despite the potential benefits of circumcision, these data are “insufficient” to recommend newborn male circumcision as part of routine medical care, and parents should weigh their religious, cultural, and personal preferences, health benefits and risks.
Other recommendations from the report include: circumcising only stable, healthy babies; providing analgesics when circumcising; educating parents on how to care for chicks, whether or not they are circumcised, etc. .
It is worth mentioning that the United States is the only Western country where circumcision is widely practiced (more than 50% of baby boys nationwide, and more than 70% in some states have the surgery soon after birth). In Australia, the UK, much of Europe and Asia, South and Central America, circumcision is uncommon.
Why in most countries do many doctors not advocate giving newborns “split foreskin”?
Internationally, most major pediatric medical and surgical specialties do not recommend circumcision in the absence of medical problems.
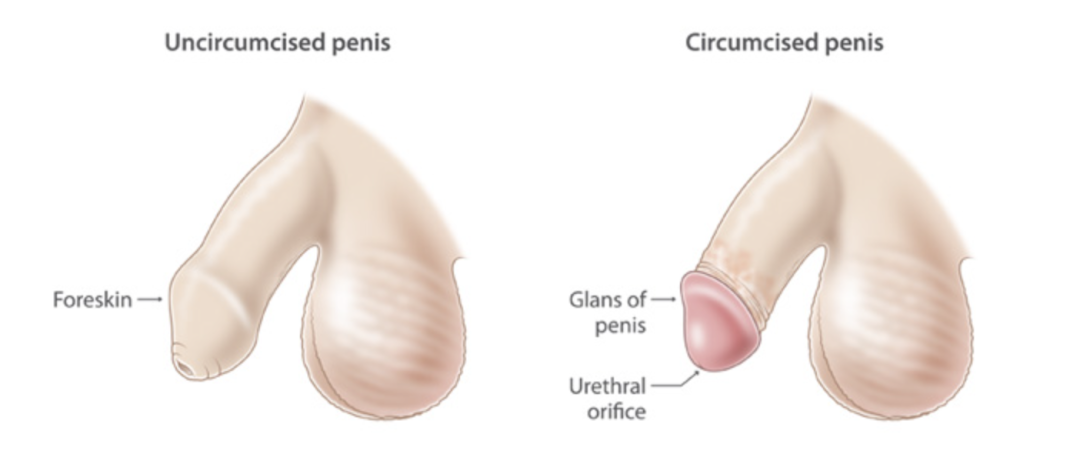
Australia does not advocate making decisions for boys as soon as they are born and permanently alter the appearance of their genitals. Yes, the glans will be permanently exposed after the circumcision scar has healed.
Unless there is a medical “really necessary reason for cutting”, the mainstream view in Australia is not to recommend cutting, even if the risk of certain diseases can be reduced. After all, surgery will inevitably have related risks.
After independently evaluating the research evidence related to circumcision, the Royal Australian College of Physicians, the Royal College of Surgeons, the Urological Society of Australia and New Zealand, and state health departments in Australia have all concluded that for non-medical reasons, including preventing future disease) the risks of circumcision outweigh the benefits.
Therefore, circumcision is not performed in public hospitals in Australia unless it is to treat conditions such as recurrent urinary tract infections or foreskin problems.
However, as the American Academy of Pediatrics points out, parents can make this decision for their children (legally), and there are reasons for circumcision or not, and it’s hard to say right or wrong.
The reasons for cutting and not cutting are listed here for your reference:
Reasons not to choose circumcision
Even when performed by an experienced doctor, circumcision can carry medical and health risks:
- Short-term problems include bleeding after surgery and going back to the hospital;
- Long-term problems include problems with the urethra and urination and concerns about the appearance of the penis, especially if too much or too little skin is removed, or more skin is removed from one side than the other;
- In rare cases, these problems can lead to damaged urethra, buried or stuck penis, gangrene, penis loss, and even death.
There are biological and ethical reasons for not opting for circumcision:
- Children grow up and they should have the right to make decisions about their bodies;
- The foreskin is a natural part of the body. It is rich in nerve endings and plays an important role in sexual sensation, sexual play and function, especially during adolescence and adulthood;
- The foreskin protects the opening of the urethra, which is very fragile early in life (it offers some hygiene risk, but also some protection);
- Why are men still allowed to be “circumcised” without medical reasons, when all forms of female circumcision are recognized by society as a whole, and the law outlaws all forms of female circumcision?
Reasons to choose circumcision
There are also several health and medical benefits of prepubertal, child circumcision:
- It can reduce the risk of urinary tract infections, especially in babies with other kidney problems;
- It prevents foreskin problems, including inflammation of the foreskin and tight foreskin during puberty.
(Parents leave this up to the child to decide.) During adolescence and adulthood, additional circumcision has the following benefits:
- It may reduce the risk of HIV and AIDS, and possibly some other sexually transmitted infections;
- It helps reduce the risk of a rare form of penile cancer in adults.
Still others may choose circumcision for religious or cultural reasons, such as Islamic practices.
When is circumcision necessary?
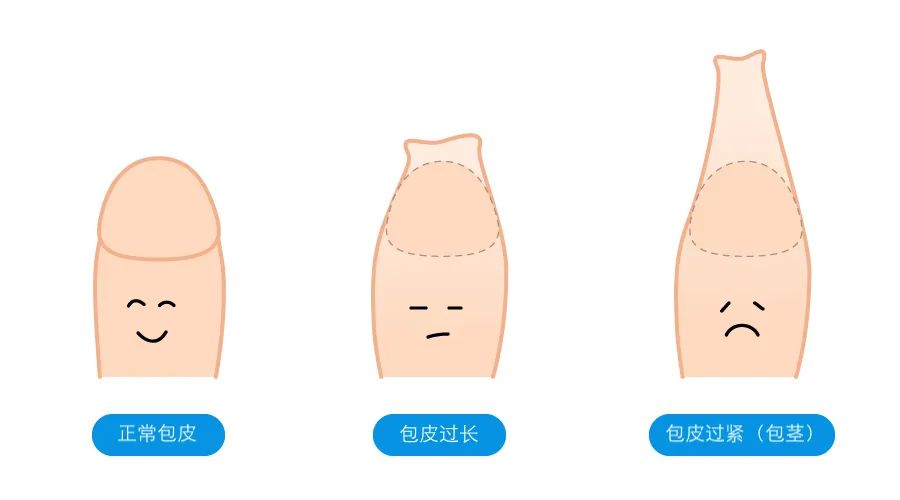
In China, most circumcisions are out of health concerns. Circumcision is performed after the age of 3, and there are two cases of circumcision: one is phimosis, and the other is the foreskin is too long.
In infants and young children, the foreskin will completely cover the glans, resulting in “physiological phimosis”, but this is a normal phenomenon, parents do not need to worry too much. Generally, after the age of 3, the glans will gradually be revealed, and 90% of the glans will be revealed naturally by the age of 7.
A domestic epidemiological survey data shows that the prevalence of phimosis in children gradually decreases with age – the incidence of phimosis in the neonatal period, infancy, early childhood, preschool and school age is 99.70%, 84.43%, respectively. %, 48.13%, 27.12% and 11.57%.
Physiological phimosis in infants and young children does not need to be treated if there is no dysuria or infection; if there is still phimosis after the age of 3, you should consult a doctor and consider whether to choose surgical or non-surgical treatment.
Studies have shown that phimosis can hinder the development of male chickens and affect sexual function. For children with phimosis, circumcision as soon as possible can help promote chicken development and improve future sexual function.
There is another situation, which is not strictly called phimosis: the glans can be exposed, but the “neckline” is a bit tight, and it can’t be squeezed on the head. Although this foreskin can be turned over, a distinct “narrow ring” can be seen, which is prone to foreskin incarceration, edema of the foreskin and swelling or bruising of the glans penis. This kind of “neckline” is a bit tight, and circumcision is also required for situations where it is easy to get stuck.
Excessive foreskin means that the foreskin covers the entire glans and urethral opening without erection, but the foreskin can still be turned up to expose the glans; or in the erect state, the foreskin needs to be turned up by hand to expose glans.
If the foreskin is too long, it is easy to hide dirt (the same is true for phimosis). Infections such as fungus will have an odor and produce a white discharge, causing redness, itching and pain in the glans. Long-term irritation of smegma also increases the risk of penile cancer.
but! The foreskin is too long does not mean that the foreskin must be circumcised, do a good job of sanitation and cleaning, and there is no repeated infection, just grow a little longer.
In a word, it can be summarized as follows: children whose phimosis has not improved after the age of 3, children whose foreskin is too long and repeatedly infected, and children whose foreskin can only be barely turned up and are prone to incarceration, need to consider circumcision.
The benefits of circumcision
What are the benefits of circumcision?
- Easy to clean and reduce the risk of urinary tract infection.
Studies have shown that after 4 weeks of circumcision, most of the pathogenic bacteria around the urethral opening in children are gone, compared to before the circumcision.
- Reduce the risk of sexually transmitted infections.
In Africa, where AIDS is high, circumcision is estimated to reduce the risk of HIV infection in men who have sex with men by 40% to 60%.
Not only that, studies have shown that circumcision can also reduce HPV infection in men and reduce the transmission of herpes simplex virus type 2 (HSV-2). For gonorrhea and chlamydia, it has not yet been found whether circumcision helps reduce the risk of both diseases.
- Reduce the risk of penile cancer
The incidence of penile cancer in the population is not very high, and thanks to the development of socio-economic level and the improvement of male hygiene habits, the incidence of penile cancer has gradually decreased in recent years (whether it is in the “enthusiasm of circumcision”. The United States, or Denmark, which doesn’t care about circumcision).
Phimosis and excessive foreskin are risk factors for penile cancer, and studies have shown that circumcision during the neonatal period can reduce the risk of penile cancer by 95% to 99%. Circumcision in childhood and adolescence reduces the risk of penile cancer by 66%. Notably, men with phimosis had 11.4 times the risk of penile cancer compared to men without phimosis!
When circumcision cannot be performed?
Circumcision cannot be performed in the following situations
- Abnormal coagulation function and obvious bleeding tendency.
- Abnormal development of the penis, such as concealed penis, webbed penis, hypospadias or epispadias, penile curvature, malrotation, etc. For example, for men with hypospadias, who need surgery to correct hypospadias in the future, they need to rely on the foreskin to extend the urethra.
- Acute foreskinitis, penile capitis, urethritis, etc., are not suitable for surgery at the stage of inflammation.
How to care after circumcision?
After circumcision, you should take care of it like this
- Wear loose, you can choose to wear special “underpants” to reduce the repeated friction between the penis and the pants. After the surgical wound is completely healed, you can change back to normal underwear.
- Pay attention to cleaning and antibacterial to avoid postoperative infection. Use antibacterial drugs to spray and change underwear every day to keep it clean. Be gentle during this process to avoid wound dehiscence.
- Pay attention to the child’s urination. Some children are afraid of urinating because of the pain after the operation. At this time, the child can be encouraged to relax, and be careful not to wet the dressing as much as possible, and wipe the urethral opening after urination.
- Properly match meals to speed up wound healing and recovery.
After reading this article, what do you think?
My thought is, unless I have to cut it, I should not decide for the child. What if the child doesn’t like it when he gets older?

